Sleeping with pain guide helps you sleep better by reducing pain, improving position, and easing night-time discomfort.
I’ve spent years helping people sleep better while living with aches, injuries, and chronic pain. This Sleeping with pain guide explains why pain disrupts sleep, what to try tonight, and how to build lasting habits that bring real relief. You’ll get clear steps, product tips, simple routines, and practical examples from real life so you can sleep with less pain and wake up feeling more like yourself.
Why pain wrecks sleep and how to think about it
Pain makes falling asleep harder and wakes you up more often. When pain spikes, stress and worry rise. That raises heart rate and keeps your brain alert. The more sleep you lose, the worse pain feels the next day. This Sleeping with pain guide helps break that cycle with small, reliable changes.
Pain affects sleep in three main ways:
- Sensory disruption — uncomfortable signals wake you.
- Emotional load — anxiety makes pain feel worse.
- Physiological change — poor sleep makes inflammation higher.
Try to treat sleep and pain together, not separately. Small wins at night often give big improvements in daytime pain.

Common causes of night pain and how to spot them
Not all pain is the same. Knowing the cause helps you pick the right fixes in this Sleeping with pain guide.
Typical causes include:
- Arthritis — stiffness and aching, often worse after rest.
- Back pain — pressure on nerves or weak muscles.
- Fibromyalgia — widespread pain and poor sleep quality.
- Injuries — acute pain in a specific area.
- Nerve pain — burning or tingling that can wake you.
- Acid reflux and breathing issues — can mimic or worsen pain.
Signs to notice:
- What time pain peaks at night.
- Which position makes it better or worse.
- Whether pain wakes you or prevents sleep onset.
- Any new medications or activities tied to flare-ups.
A clear diary for a week helps identify triggers. Note time, position, pain level, and sleep hours.
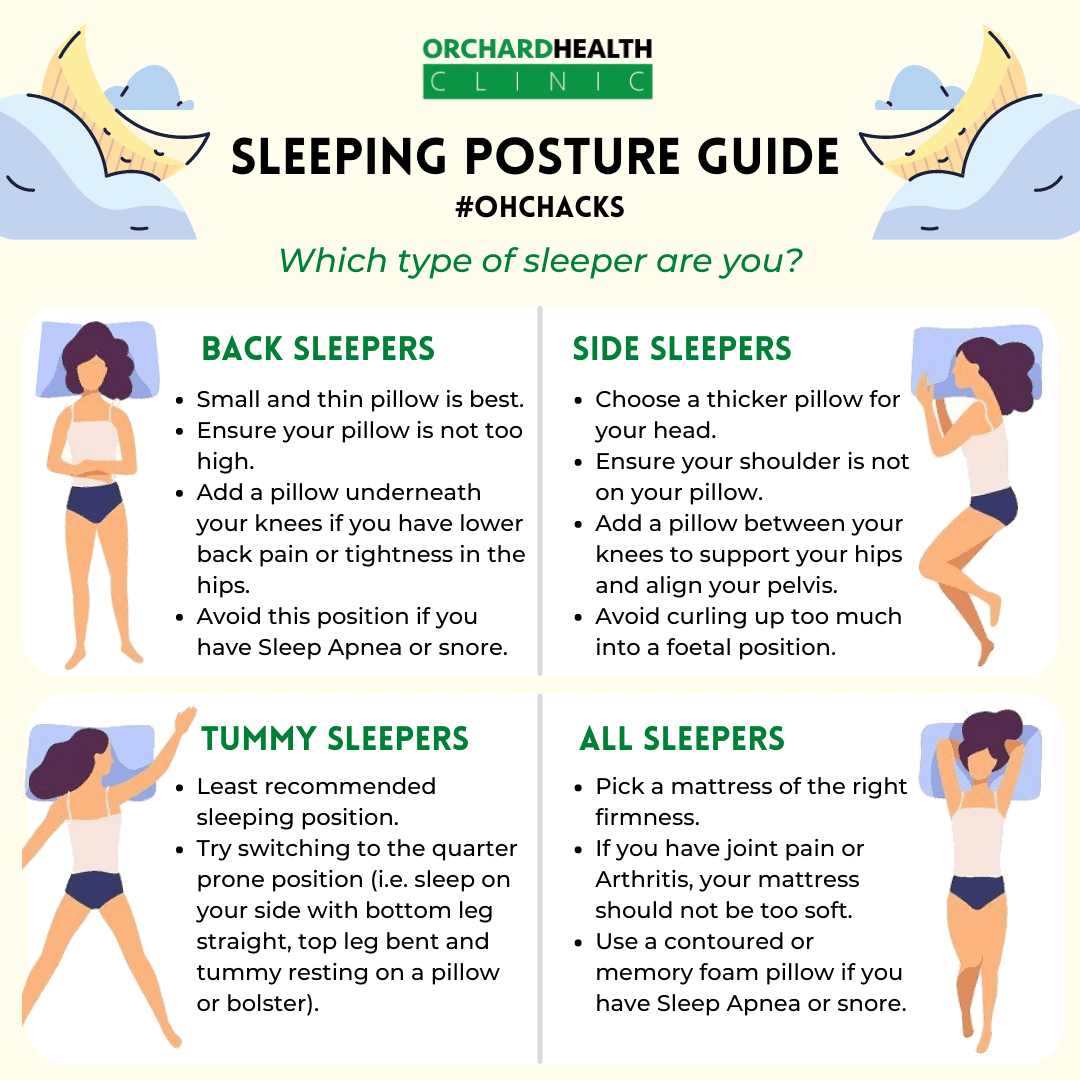
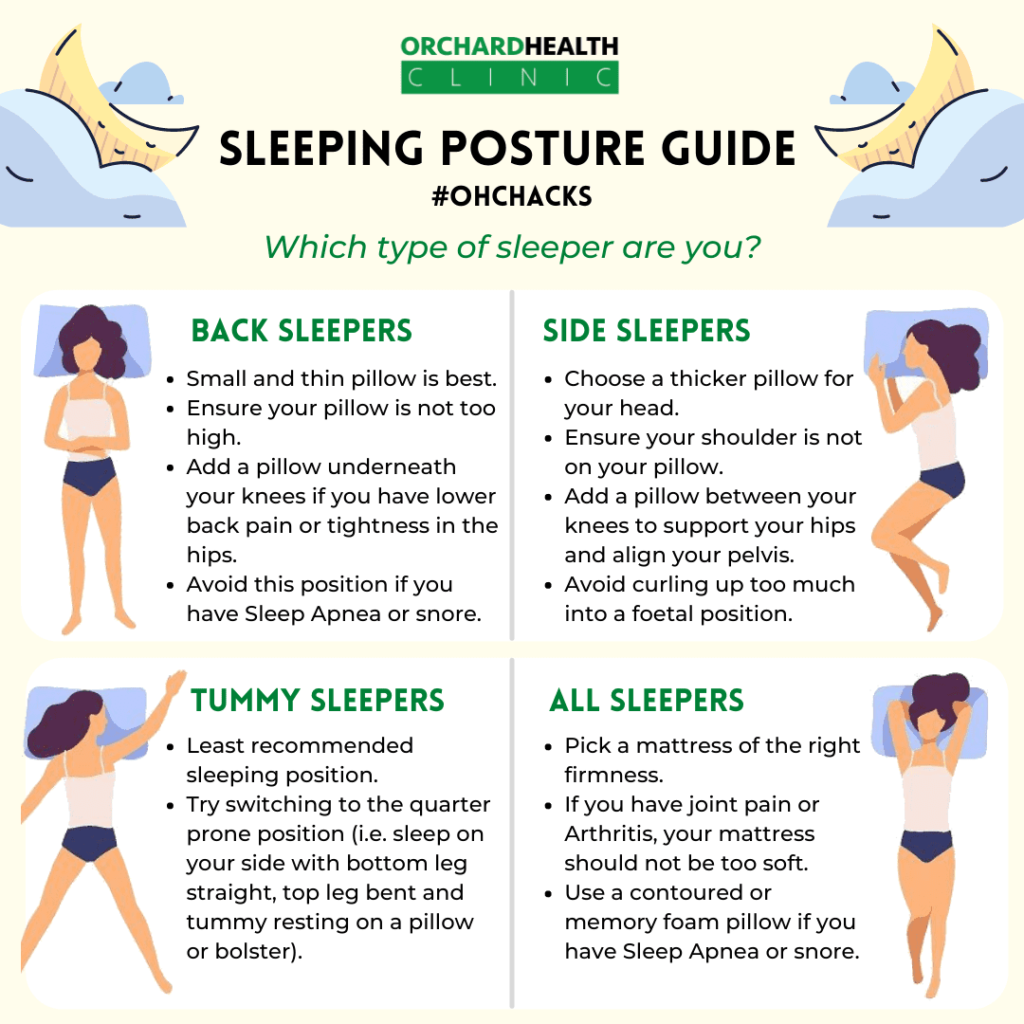
Best sleep positions for different pains
The right position can reduce pressure and improve rest. This part of the Sleeping with pain guide gives simple swaps you can try tonight.
Back pain
- Lie on your back with a pillow under your knees to keep a neutral spine.
- If back pain is lower, place a small rolled towel under your lumbar curve.
Neck pain
- Use a medium loft pillow that supports the natural curve of the neck.
- Try a cervical pillow or a rolled towel inside the pillowcase.
Hip pain
- Sleep on the non-painful side with a thick pillow between knees to align hips.
- On your back, place a pillow under both knees.
Shoulder pain
- Sleep on the opposite side or on your back with a pillow supporting the affected arm.
- Avoid sleeping on the painful shoulder.
Stomach sleepers
- Shift toward back sleeping if possible; place a thin pillow under pelvis to reduce lower back strain.
Small changes in position often reduce night-time pain quickly. Test one change at a time to see what helps.

Mattress, pillows, and bedding: what to choose
Your bed matters. The right mattress and pillows relieve pressure points and support alignment. The Sleeping with pain guide emphasizes comfort, not fashion.
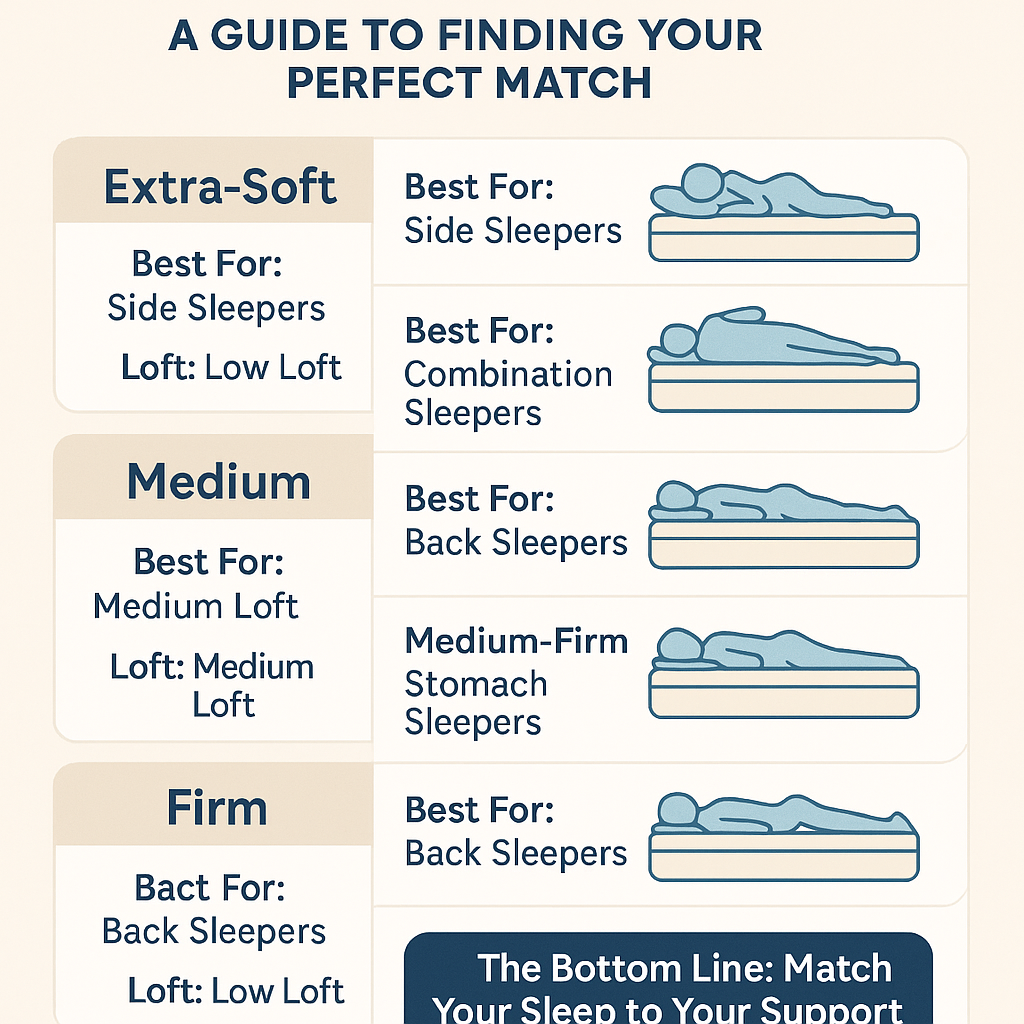
Mattress tips
- Medium-firm mattresses are best for most people with back or joint pain.
- Memory foam contours pressure but can trap heat; choose cooling foams if you sleep hot.
- Hybrid mattresses balance support and contouring for better spinal alignment.
- Replace pillows every 1–2 years or when they lose shape.
- Choose pillow loft by your sleep position: higher for side, medium for back, low for stomach.
- Try specialty pillows for neck pain or shoulder relief.
Bedding and temperature
- Keep bedroom cool; lower temperature helps deeper sleep and eases pain.
- Use breathable sheets and light blankets to avoid overheating, which can amplify pain.
Test at home for a few nights before switching expensive items. Many brands offer trial periods for this reason.

Evening routines and quick pain-relief strategies
A calm pre-sleep routine reduces pain sensitivity. This section of the Sleeping with pain guide gives simple nightly steps you can follow.
Wind-down routine
- Stop screens 30–60 minutes before bed.
- Do gentle stretching or yoga for 10 minutes.
- Use deep breathing or a short guided meditation to lower stress.
Heat and cold therapy
- Use a heating pad on muscles for 15–20 minutes to ease tightness.
- Apply ice to reduce inflammation after injury for 10–15 minutes.
Topical treatments and OTC options
- Topical analgesics can help localized pain without systemic effects.
- Over-the-counter pain relievers may help short-term; follow dosing and doctor advice.
Night-time aids
- Consider using a support brace or compression sleeve overnight if recommended.
- Weighted blankets may help anxiety but can increase pressure on sore joints — use cautiously.
I once used a 10-minute pre-sleep stretch and a heating pad to sleep through a week-long flare. That small routine cut my night wakings in half.

Medications, therapies, and when to see a doctor
This Sleeping with pain guide reviews medical options and when to seek professional care.
When to see a doctor
- Pain that worsens or limits mobility.
- New numbness, tingling, or weakness.
- Unexplained weight loss, fever, or systemic symptoms.
Medical options
- Prescription pain meds for short-term control, under guidance.
- Physical therapy for strengthening and posture.
- Cognitive behavioral therapy for insomnia (CBT-I) to treat sleep disruption linked to pain.
- Interventional procedures for specific conditions when conservative care fails.
Always discuss long-term medication use with a clinician. Non-drug options often produce durable benefits with fewer risks.
Lifestyle habits that reduce pain and improve sleep
Good daytime habits make night-time better. This part of the Sleeping with pain guide focuses on small, doable changes.
Daily movement
- Move regularly; avoid long periods of sitting.
- Mix gentle cardio, strength, and flexibility exercises.
Nutrition and hydration
- Eat balanced meals and avoid heavy late-night snacks.
- Reduce alcohol and caffeine near bedtime.
Stress and mood
- Manage stress with short, daily practices like walking or breathwork.
- Seek social support or counseling when pain leads to low mood.
These habits cut pain flare frequency and improve sleep quality over weeks and months.

Personal experience and practical tips I use
I’ve coached dozens of people through painful nights. Here are tips that worked most reliably for real people.
What helped my clients most:
- A consistent sleep-wake time, even on weekends.
- A simple 10-minute stretch and heat routine before bed.
- Swapping pillows to match sleep position — often a single change did the trick.
- Keeping a pain-sleep diary for two weeks to identify triggers and solutions.
Mistakes to avoid:
- Relying on quick fixes like heavy sleeping pills without addressing habits.
- Changing multiple things at once; you can’t tell what helped.
- Ignoring new or worsening symptoms that need a clinician.
These real-world steps form the core of my Sleeping with pain guide advice. They’re low-cost and low-risk, and many people see clear gains within days.
Action plan: a 7-day trial to sleep with less pain
Try this week-long plan from the Sleeping with pain guide to test what works for you.
Day 1
- Note baseline sleep and pain levels. Adjust one pillow.
Day 2
- Add a 10-minute stretch and 15-minute heating pad before bed.
Day 3
- Swap mattress topper or change sleeping position if possible.
Day 4
- Remove screens 60 minutes before bed and do calming breathing.
Day 5
- Add short walk or light exercise in the morning.
Day 6
- Try a topical analgesic or compression wrap if helpful.
Day 7
- Review your diary. Keep what improves sleep and drop what doesn’t.
Small, steady changes often yield the best results. This trial helps isolate effective strategies.
Frequently Asked Questions of Sleeping with pain guide
What immediate steps can I take tonight to reduce pain and sleep better?
Start with position changes, a short stretch, and heat for tight muscles. Lower room temperature and avoid screens before bed.
Can changing my mattress help with chronic pain?
Yes, a supportive medium-firm mattress often reduces joint and back pain. Try a trial period to confirm improvement.
Are sleeping pills a good long-term solution for pain-related insomnia?
Sleeping pills may help short-term but are not ideal for long-term use. Combine them with behavioral changes and medical advice.
How long before I see improvements using this Sleeping with pain guide?
Some people notice changes in a few nights; others take weeks. Consistency in routines and posture matters most.
When should I consult a specialist about night-time pain?
See a doctor if pain worsens, if you have new numbness or weakness, or if pain severely limits daily life. Early evaluation helps get better outcomes.
Conclusion
This Sleeping with pain guide gives practical, step-by-step ways to reduce night pain and improve sleep. Start small: adjust one thing, track results, and build routines that stick. Use the 7-day plan, try position and bedding changes, and seek medical help for worrying symptoms. Take action tonight — test one change and note the difference. If this helped, subscribe for more guides or leave a comment about what worked for you.

Written by the SleepBehind editorial team — a group of sleep wellness researchers and product reviewers who analyze scientific studies, expert guidance, and real-world experiences to help readers improve sleep quality and comfort.