Sleep with a yeast infection by keeping the area cool, dry, treated, and wearing breathable sleepwear.
I’ve helped many people manage nighttime discomfort from yeast infections, and I know how disruptive itch and burning can be to sleep. This guide on how to sleep with yeast infection explains clear, practical steps you can use tonight to reduce itching, stay comfortable, and support healing. I combine clinical tips, easy home measures, and real-life advice so you can rest better while treating the infection.
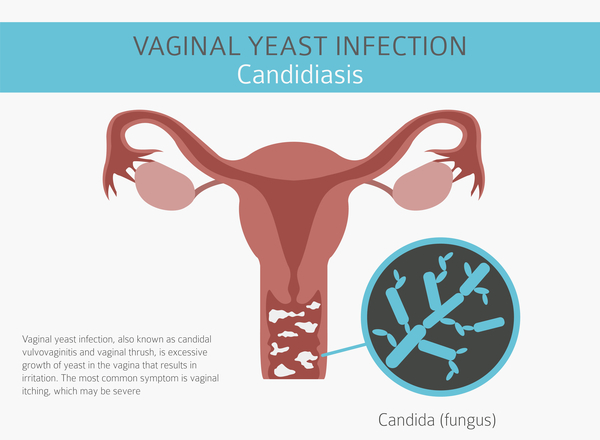
What is a yeast infection and why it affects sleep
A yeast infection is an overgrowth of Candida fungi on skin or mucous membranes. It commonly affects the vulva and vagina, but it can also appear on the skin folds. The infection causes itching, burning, and irritation that get worse at night for many people.
Nighttime symptoms often feel worse because heat and moisture build up while you sleep. Lying still can trap warmth and reduce airflow. These conditions make itch and irritation harder to ignore and make falling or staying asleep difficult.

Symptoms that interfere with sleep
Common symptoms that disturb sleep include intense itching, burning during urination, and a raw or sore feeling. Some people report worse itchiness after a hot shower or after exercise. Disrupted sleep can cause fatigue and worsen mood the next day.
If discharge or odor is present, you may wake to check or change clothes. These repeated awakenings reduce deep restorative sleep. Addressing the root cause and the immediate symptoms can help you sleep more soundly.
Practical nighttime steps: how to sleep with yeast infection
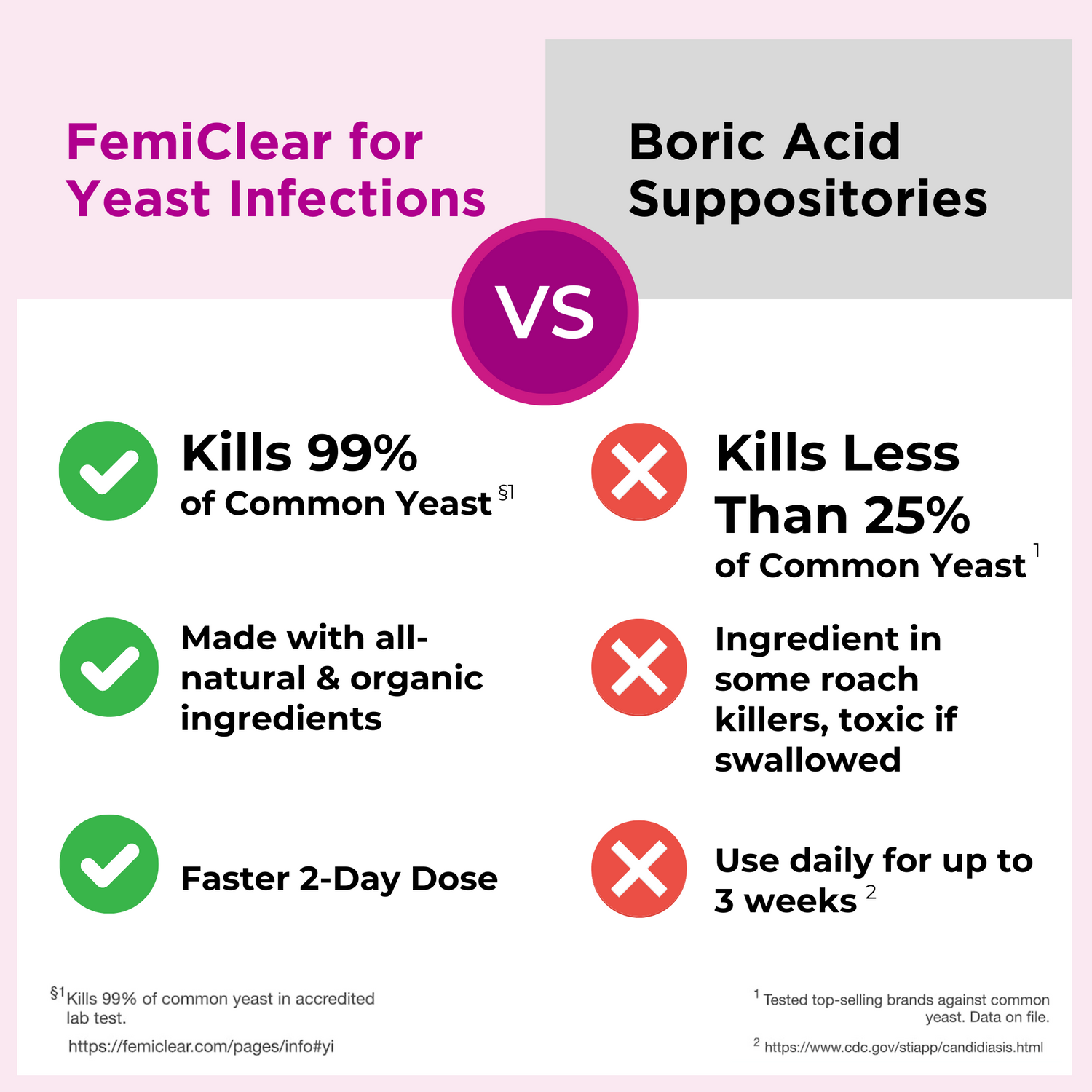
Take antifungal treatment as directed before bed to let medication work overnight. Over-the-counter creams or suppositories applied at night can reduce fungal load while you sleep. If you use oral antifungal medication, follow your provider’s timing instructions to maximize effect.
Keep the genital area dry and cool before bed. Pat the area gently with a clean towel and allow a few minutes of air-drying. Avoid tight underwear and choose breathable sleepwear made of cotton or moisture-wicking fabric.
Apply soothing, non-irritating relief if you need quick comfort. A cool compress for 10 minutes can reduce burning and soothe inflammation. Avoid home remedies that sting, like undiluted vinegar or harsh soaps, which can worsen symptoms.
I once advised a friend to switch to nightly topical treatment and breathable shorts. She reported falling asleep faster within two nights. Simple, consistent steps often give quick relief.

Bedtime hygiene and clothing
Wear loose, breathable sleepwear to promote airflow. Choose 100% cotton or moisture-wicking fabrics that move moisture away from skin. Sleep without underwear if that feels comfortable and reduces warmth.
Change sheets and pajamas often during flare-ups. Clean bedding reduces trapped yeast and keeps you feeling fresher. Use gentle, fragrance-free detergent to avoid irritation.
Avoid creams or powders with fragrances at night. Products with perfumes or strong chemicals can inflame sensitive skin. Stick to plain, approved antifungal creams or prescribed options.
:max_bytes(150000):strip_icc()/GettyImages-979320038-4f24163c17a844c1817df3daf30fc6f4.jpg)
Sleep positions, bedding, and cooling strategies
Choose positions that reduce friction on irritated skin. Sleeping on your back with legs slightly apart can limit rubbing. Side sleeping with a small pillow between the knees may also help reduce pressure.
Cool the bedroom to reduce sweating. A lower room temperature decreases warmth and moisture buildup. Use a fan or breathable sheets to keep air moving.
Try moisture-wicking mattress protectors and breathable bedding. These items help reduce trapped moisture that feeds yeast growth. Replace synthetic sheets with natural fiber options when possible.

Over-the-counter and prescription treatments to use before bed
OTC antifungal creams, ointments, and suppositories can be applied at night for continuous action. Read the label for frequency and duration. Most topical treatments are safe and effective for short-term use.
Oral antifungal pills are an option for recurrent or severe infections. These are usually taken once, or as prescribed over several days. Discuss with a healthcare provider before starting oral medication.
Avoid combining multiple topical treatments without advice. Using too many products can irritate the skin and delay healing. If symptoms persist after a full course, seek medical evaluation.

When to see a healthcare provider
See a provider if symptoms are severe, recurrent, or do not improve after treatment. Extreme pain, fever, or unusual discharge warrant prompt care. Recurrent infections may need testing or different medications.
If you are pregnant, consult your provider before using oral antifungals. Some treatments are not recommended during pregnancy. A clinician can recommend safe alternatives.
Be honest about symptoms and treatment history. Accurate information helps your provider choose the right plan and reduces time to relief.

Preventing recurrence and long-term sleep improvements
Keep the genital area dry and clean as part of daily routine. Change out of sweaty clothes promptly after exercise. Avoid long baths or hot tubs that can change vaginal pH.
Limit tight clothing and synthetic underwear during the day. Choose breathable fabrics and avoid prolonged dampness. Consider probiotics or dietary adjustments if recurrence is a pattern, after discussing with a provider.
Track triggers that precede flare-ups, such as antibiotics, stress, or specific products. Knowing what triggers your infections helps you avoid them and get better sleep overall.

Frequently Asked Questions of how to sleep with yeast infection
How long should I expect sleep disruption from a yeast infection?
Most people see symptom relief within a few days of starting effective topical treatment, with sleep improving as symptoms lessen. Severe or recurrent infections may take longer and need medical care.
Can I sleep without underwear when I have a yeast infection?
Yes. Sleeping without underwear can improve airflow and reduce moisture, which often helps reduce itching and speed healing. Make sure bedding and pajamas are clean and breathable.
Will a cold compress at night help with itching?
A cold compress can temporarily relieve burning and itch for 10 to 15 minutes. Use a clean cloth and avoid applying ice directly to the skin to prevent further irritation.
Is it safe to use OTC creams every night?
Follow the product directions; many OTC antifungal creams are meant to be applied once or twice daily for a set number of days. Overuse can irritate skin, so consult a provider if symptoms persist.
When should I see a doctor for nighttime symptoms?
See a doctor if symptoms worsen, do not improve after treatment, or if you have fever, severe pain, or unusual discharge. Recurrent infections also merit medical evaluation.
Conclusion
Sleeping well while you treat a yeast infection is possible with simple, consistent steps. Use the right treatment, keep the area cool and dry, wear breathable sleepwear, and address triggers to reduce flare-ups. Start tonight by applying treatment before bed and adjusting sleepwear or bedding for airflow.
Take action now: try one new bedtime change tonight and track how it affects your sleep. If symptoms do not improve, consult a healthcare provider for tailored care and faster relief.

Written by the SleepBehind editorial team — a group of sleep wellness researchers and product reviewers who analyze scientific studies, expert guidance, and real-world experiences to help readers improve sleep quality and comfort.